What is Gastro and Hepatobiliary?
Gastroenterology is the branch of medicine focused on the digestive system and its disorders. The specialist who deals with this disorder is called a Gastroenterologist.Hepatobiliary is the branch of medicine that focuses on the hepatobiliary system i.e. the liver gallbladder and bile ducts. Hepatobiliary disease encompasses any condition affecting the hepatobiliary system that disrupts its normal operations. These disorders can vary in severity, from mild infections or scarring to more severe illnesses such as cancer. The specialist that deals with this disorder is called a hepatobiliary surgeon.
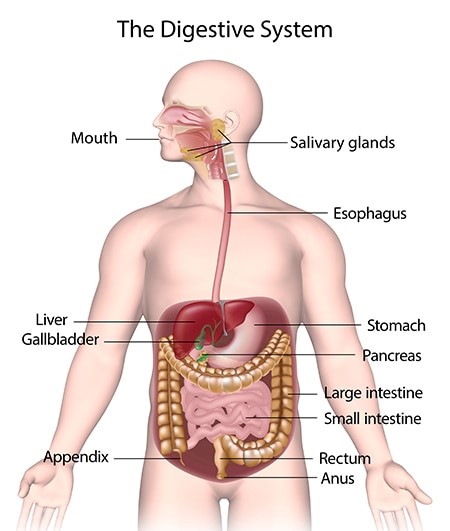
What is the digestive system?
The digestive system is a web of organs designed to assist in the digestion and absorption of nutrients from food. This system consists of the gastrointestinal (GI) tract (mouth, esophagus, stomach, small intestine, large intestine and anus) and the biliary system. The biliary system, on the other hand, is comprised of three organs (liver, gallbladder, pancreas and bile ducts) that transport bile and enzymes to the GI tract via bile ducts.
Who is in the Multidisciplinary Team?
A multidisciplinary team of specialists, including surgeons, radiologists, interventionists, endoscopists, hepatologists, anesthesiologists, nutritionist, psychologist and pathologists, adopts a patient-centered methodology to provide treatment for individuals diagnosed with malignant tumors affecting the stomach, pancreas, gallbladder, liver, bile duct, and duodenum.Conditions and Disorders
Which parts are affected by the digestive system?
Various temporary conditions and chronic diseases can impact the digestive system. Occasional issues like constipation, diarrhea, or heartburn are normal. Some of the conditions include:- Problems with the Oesophagus – including acid reflux, achalasia, e.g. difficulty in swallowing may suggest esophageal growth which may disrupt feeding which may need a PEG tube
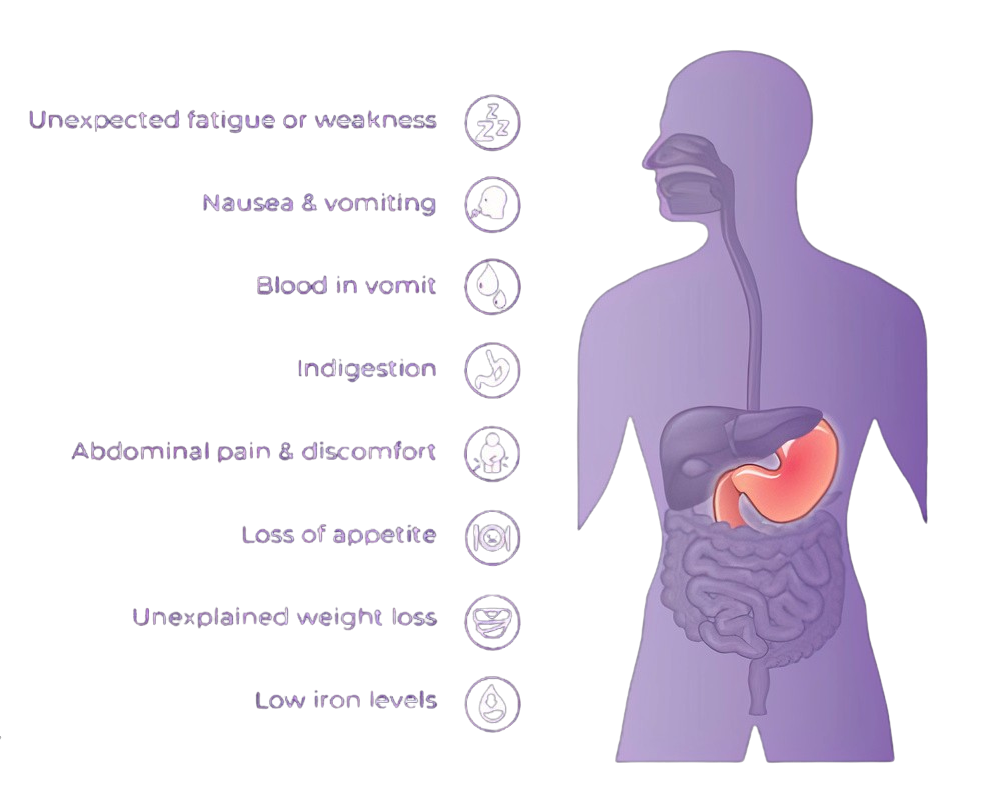
- Problems with the stomach – including gastro paresis, stomach ulcers, and stomach cancer, acid reflux / GERD.
- Problems with the gallbladder – including gallstones. and inflammation of gall bladder, gall bladder cancers, blocked biliary tree which may require an ERCP with stenting.
- Problems with the pancreas – including pancreatitis and pancreatic cancer
- Problems with the liver – including liver cysts and liver cancer
- Problems with the intestines – including coeliac disease, dysentery, Hirschsprung's disease, irritable bowel syndrome (IBS), and ulcerative colitis, diverticulitis, colon cancer, and polyps
- lems with the rectum – including, anal fissure, anal fistula, and hemorrhoids
- lems with the system as a whole – including Crohn’s disease
- es generally related to dietary problems – including constipation, indigestion, flatulence, food intolerances, and lactose intolerance.
Common digestive system diseases (gastrointestinal diseases) and disorders include:
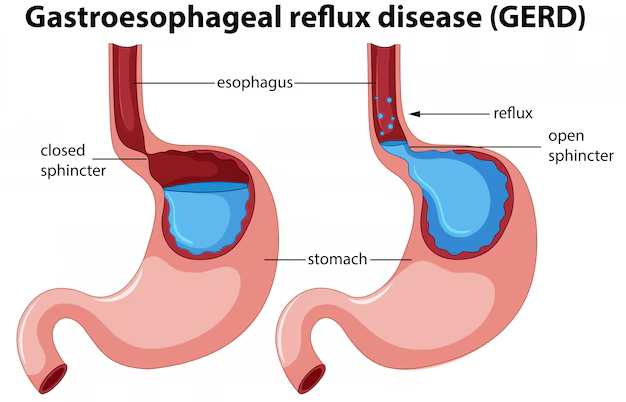
- GERD (chronic acid reflux): GERD, also known as gastroesophageal reflux disease or chronic acid reflux, is characterized by the frequent backflow of stomach acid into the esophagus.
- Irritable bowel syndrome (IBS): IBS is a disorder characterized by irregular contractions of the colon muscles. Individuals with IBS may suffer from frequent gas, as well as abdominal pain and cramping.
- Lactose intolerance: Individuals who suffer from lactose intolerance have difficulty digesting lactose, which is the main sugar present in milk and dairy items.
- Diverticulosis and diverticulitis: Diverticulosis and diverticulitis are a pair of conditions that manifest in the large intestine, also known as the colon. They both exhibit diverticula as a common characteristic, which are pockets or bulges that develop in the colon wall.
- GI Cancers: Some of the most prevalent digestive system cancers are esophageal cancer, gastric (stomach) cancer, colon and rectal (colorectal) cancer, gall bladder cancers, pancreatic cancer, and liver cancer.
- Crohn’s disease: Crohn's disease is a chronic type of inflammatory bowel disease (IBD) that causes inflammation in the digestive tract.
- Stomach flu (gastroenteritis): The stomach flu, typically caused by a virus or ameba, is an infection affecting the stomach and upper portion of the small intestine. It commonly resolves within a week, with millions of individuals experiencing this illness annually.
- Ulcers: An ulcer is a lesion that forms on the mucous membrane of the esophagus, stomach, or small intestine. May be caused by Helicobacter pylori (H. pylori) and prolonged use of medications like ibuprofen.
- Gallstones: Gallstones are tiny solid particles created from digestive fluid that develop in the gallbladder, a small organ located beneath the liver.
- Cholecystitis: Swelling or inflammation of the gall bladder. A painfulcondition that may lead to dangerous complications
-
Hernia: A hernia arises when an internal component of the body protrudes through a weakness in the muscular or surrounding tissue wall. Types of Hernia are:

- Inguinal Hernia - the intestines protrude through a vulnerable area or rupture in the lower abdominal wall
- Hiatal Hernia- the upward displacement of a portion of the stomach through the diaphragm into the thoracic cavity
- Umbilical Hernia - intestines protrude through the abdominal wall in the vicinity of the navel. It can affect children and babies

Common Signs & Symptoms of the Various Conditions Above
- Constipation: Constipation typically occurs when bowel movements are less frequent than usual, resulting in dry, hard stool that is difficult and painful to pass.
- Diarrhea: Diarrhea occurs when an individual experiences loose or watery bowel movements. It can be triggered by various factors, such as bacteria, although at times the exact cause remains unidentified.
- Heartburn: Despite the name is not related to the heart burn is a digestive problem. It is characterized by a painful burning sensation in the chest that may extend to the neck and throat. This occurs when acidic stomach juices reflux back into the esophagus.
-
Hemorrhoids: Hemorrhoids are enlarged, swollen veins that develop both internally and externally around the anus and rectum. They have the potential to be painful, cause discomfort, and result in rectal bleeding.
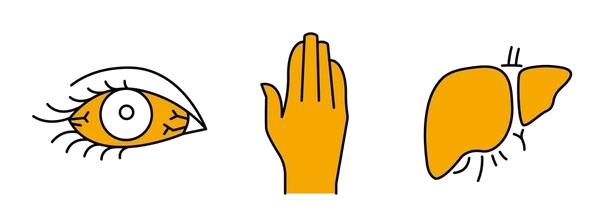
- Yellowing/itchy skin: Jaundice, characterized by a yellowish tint to the skin and eyes, arises from an accumulation of excess bilirubin in the bloodstream. This yellow discoloration may signal a range of underlying health issues related to the liver, including hepatitis, liver cirrhosis, or obstructive jaundice.

- Stomach Cancers:
-
Flatulence/Bloating: Bloating and flatulence are common gastrointestinal (GI) symptoms experienced by individuals across various age groups. Consuming food rapidly can result in the ingestion of air with each bite, potentially leading to bloating over time.
Additionally, certain food intolerances, such as those related to lactose or fructose, may contribute to this condition. Foods rich in raffinose, a complex sugar known to produce gas, are also culprits.
Examples of such foods include cruciferous vegetables like broccoli, cabbage, Brussels sprouts, asparagus, cauliflower, and various types of beans.
Investigations
A. Common Lab works.
- Complete Blood Count: Used to rule out anemia, bacterial and viral infections
- Helicobacter Pylori: to determine the presence of the bacteria called Helicobacter Pylori. This bacterium is a causative agent for peptic and duodenal ulcers.
- Fecal occult blood or fecal immunochemical test. This test checks for microscopic amounts (occult) of blood in the stool. A very small amount of stool is placed on a test card. The stool is then tested in the healthcare provider's office or sent to a lab.
- Stool culture. This test checks for abnormal bacteria in the digestive tract that may cause diarrhea and other problems. A small sample of stool is collected and sent to a lab. In 2 or 3 days, the test will show if abnormal bacteria are present.
- Breath tests. These can help diagnose several digestive disorders. These include stomach bacteria (H. pylori), poor digestion of sugars (for example, lactose or milk sugar), bacterial overgrowth, and delayed stomach emptying (gastroparesis).
- Kidney Function test (UEC’s): To determine if the kidney is excreting waste products of metabolism.
- Liver Function test: To measure several enzymes made by the liver. Many different parameters such as ALP, AST, ALK , bilirubin etc. are measured to diagnose infection, blockage in biliary tree and so on
- CRP: Is a protein made by the liver. It measures the C-reactive protein in the blood indicating the presence of inflammation.
- PT INR: Prothrombin, produced by the liver, is a vital protein involved in the blood clotting process. Along with other clotting factors, it plays a crucial role in forming blood clots to stop bleeding caused by cuts or injuries
B. Imaging test
- Diagnostic Gastroscopy/OGD: Non- Surgical procedure done to look inside the Oesophagus, stomach and duodenum using a flexible tube with a camera at one end inserted through the mouth, under sedation
- Diagnostic Colonoscopy: Non-surgical procedure done to look inside (visually) the large intestine (colon) using a flexible tube with a tiny camera at one end inserted through the anus, under sedation.
- Biopsy: In a biopsy, a small sample of tissue is extracted via scope or needle from the digestive system and analyzed microscopically for the presence of cancerous cells.
- CT scan. This imaging test uses X-rays and a computer to make detailed images of the body. A CT scan shows details of the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays.
- Barium enema - It looks at the rectum, the large intestine, and the lower part of the small intestine. Barium is given into the rectum as an enema. An X-ray of the abdomen shows strictures (narrowed areas), obstructions (blockages), and other problems.
- MRI scan. This test uses a combination of large magnets that take a series of pictures of the inside of the body using a magnetic field and radio waves. The computer enhances the pictures. The test is painless. Used to give detailed images of internal body organs.
- Magnetic resonance cholangiopancreatography (MRCP). This test uses MRI to view the bile ducts. The machine uses radio waves and magnets to scan internal tissues and organs.
- Barium swallow - In this test, you are given small amounts of a liquid containing barium to drink with a bottle, spoon, or cup. A series of X-rays is taken to see what happens as you swallow the liquid.
- Ultrasound. This imaging test uses high-frequency sound waves and a computer to make images of blood vessels, tissues, and organs. Ultrasounds are used to view internal organs as they function. It can also assess blood flow through various vessels.
Prevention of Gastro & Hepatobiliary Diseases
How can I keep my digestive system healthy?
The following are ways to keep your digestive system healthy:
- Drink water often:Water helps the food you eat flow more easily through your digestive system. Low amounts of water in your body (dehydration) is a common cause of constipation.
- Include fiber in your diet: Fiber is beneficial to digestion and helps your body have regular bowel movements. Be sure to incorporate both soluble and insoluble fiber into your diet.
- Eat a balanced diet: Be sure to eat several servings of fruit and vegetables every day. Choose whole grains over processed grains and try to avoid processed foods in general. Choose poultry and fish more often than red meat and limit all deli (processed) meats. Limit the amount of sugar you consume.
- Eat foods with probiotics or take probiotic supplements: Probiotics are good bacteria that help fight off the bad bacteria in your gut. They also make healthy substances that nourish your gut. It can be especially helpful to consume probiotics after you have taken an antibiotic because antibiotics often kill both bad and good bacteria in your gut.
- Eat mindfully and chew your food: Eating slowly gives your body time to digest your food properly. It also allows your body to send you cues that it is full. It is important to chew your food thoroughly because it helps to ensure your body has enough saliva (spit) for digestion. Chewing your food fully also makes it easier for your digestive system to absorb the nutrients in the food.
- Exercise: Physical activity and gravity help move food through your digestive system. Taking a walk, for example, after you eat a meal can help your body digest food more easily.
- Avoid alcohol and smoking: Alcohol can increase the amount of acid in your stomach and can cause heartburn, acid reflux and stomach ulcers. Smoking almost doubles your risk of having acid reflux. Research has shown that people who have digestive issues that quit smoking have improved symptoms.
- Manage your stress: Stress is associated with digestive issues such as constipation, diarrhea and IBS.

Treatment of Gastroinstitinal Conditions
A. Medications:
- Antacids and Proton Pump Inhibitors (PPIs): for the management of GERD, as they help to decrease the production of stomach acid.
- Anti-Inflammatory Drugs: In the treatment of Inflammatory Bowel Disease (IBD), anti-inflammatory agents such as mesalamine or corticosteroids are utilized to manage inflammation.
- Anti-nausea: Medications prescribed to suppress nausea and vomiting e.g Domperidone, Ondansetron, Metoclopramide.
- The Helicobacter pylori eradicative agents: The agents used for the eradication of Helicobacter pylori are administered in conjunction with antibacterial medications to address H. pylori infections.
- Bile agents solubilize cholesterol are utilized for non-calcified small stones that may not require surgical intervention. These agents function by decreasing the liver's synthesis of cholesterol or by inhibiting its absorption in the gastrointestinal tract.
- The laxatives: serve a beneficial purpose in alleviating constipation by enhancing the frequency of bowel movements or facilitating the passage of stool. This can be achieved using stool softeners or lubricants.
- Antibiotics: work to cure some forms of bacterial gastroenteritis.
- Probiotics: Probiotics offer several advantageous effects pertinent to the treatment and prevention of gastroenteritis, including a decrease in the invasion and colonization of the intestines by pathogenic organisms, an alteration of the host's immune response, and a reduction in intestinal pH.
B. Surgery
In certain situations, surgical intervention is essential for the management or treatment of gastrointestinal conditions. For instance:
- Cholecystectomy: This procedure involves the surgical excision of the gallbladder to address the presence of gallstones.
- Colectomy:In instances of severe ulcerative colitis or diverticulitis, it may be necessary to remove a segment of the colon.
- Ileostomy or Colostomy: In critical cases of inflammatory bowel disease, diverticulitis, or trauma, these surgeries create a stoma to facilitate waste elimination, circumventing the compromised region.
- Nissen Fundoplication is a surgical intervention designed to address gastroesophageal reflux disease (GERD). In this procedure, the upper section of the stomach, known as the fundus, is wrapped and sutured around the lower esophageal sphincter, which is a muscular valve located at the base of the esophagus.

C. Procedures:
- ERCP(Endoscopic Retrograde Cholangiopancreatography): it is a procedure done to treat and diagnose problems in the gallbladder, pancreas, bile ducts and liver.
- Diagnostic Gastroscopy/OGD : Non- Surgical procedure done to look inside the Oesophagus, stomach and duodenum using a flexible scope.
- Diagnostic Colonoscopy : Non-surgical procedure done to examine the large intestine (colon).
- Percutaneous Endoscopic Gastrostomy (PEG) tube Placement is a feeding tube surgically placed through your abdomen into your stomach.
- Therapeutic Endoscopy/OGD : procedures provide treatment that is carried out via the endoscope.
- Duodenoscopy: procedure that involves looking at the upper part of the gut which includes the Oesophagus (food pipe), stomach and the first part of your small bowel (duodenum) with a narrow flexible tube called a gastroscope.
- Polypectomy: is the removal of an abnormal growth of tissue called a polyp
- Gastric banding: The surgeon places a band around the upper part of your stomach to create a small pouch to hold food.






















